
By Dr Azizur Rehman, Muhammad Hamza, Waqas Haider, and Qosain Ahmad
University of Veterinary and Animal Sciences Lahore, Sub-campus Jhang
Salmonella species, which are gram-negative, flagellated, motile bacilli and facultative intracellular pathogens, are globally significant, causing approximately 1.3 billion cases of disease annually in both humans and animals, with most strains being non-lactose fermenters, although lactose-fermenting strains do occasionally emerge; evidence indicates that Salmonella Typhi, whose ancestor existed between 15,000 to 150,000 years ago, dispersed worldwide during a time when humans were still hunters.
Salmonella infections are a major contributor to high morbidity rates, particularly in underdeveloped regions characterized by poor hygiene standards. Clinical manifestations in humans range from typhoid fever, caused by Salmonella Typhi and Salmonella Paratyphi, to various syndromes such as diarrheal diseases linked to numerous non-typhoidal Salmonella serovars (NTS).
Salmonella encompasses over 2500 serovars of S. enterica, categorized by somatic (O) and flagellar (H) antigens, occasionally with capsular (Vi) antigens. These serovars span six subspecies: enterica, salamae, arizonae, diarizonae, houtenae, and indica, with S bongori having no subspecies. Further differentiation into serovars is based on flagellar, carbohydrate, and lipopolysaccharide (LPS) structures, according to the Centers for Disease Control (CDC).
Salmonella serotypes are globally distributed, infecting mammals, birds, and reptiles, primarily excreted through feces. The primary route of infection is ingestion, but mucosal contact with the upper respiratory tract and conjunctiva can also lead to infection. These organisms can be found in water, soil, animal feeds, and raw meat, with feces as the primary source of environmental contamination. Subspecies S. enterica serotypes Typhi and Paratyphi cause enteric fever, while NTS often result in invasive presentations associated with significant mortality.
The transmission routes of Salmonella infection in humans encompass several pathways. Firstly, ingestion stands out as the primary route through which individuals contract Salmonella. This typically occurs when individuals consume contaminated food or water, which may contain these harmful bacteria.
Another route of transmission involves close contact with infected animals. This is particularly relevant for individuals who work with or have direct contact with animals that may carry Salmonella, such as poultry or reptiles.
In addition to these routes, human-to-human transmission of Salmonella is possible, albeit less common. It can occur when an infected individual passes on the bacteria to others through contact or through contaminated items and surfaces.
Furthermore, Salmonella organisms are not confined solely to humans and animals. They can also be found in various environmental sources, including water, soil, animal feeds, raw meat, vegetable material, and feces. This underscores the importance of thorough food safety practices and proper hygiene to prevent Salmonella infections and outbreaks.
The pathogenesis of Salmonella infection is influenced by factors such as bacterial dose, host age, immune status, and serovar. Typically, infection occurs through the ingestion of contaminated food or water. Host-adapted serovars tend to cause more severe disease, with endemic occurrences on farms but low clinical infection rates.
Virulence in Salmonella serotypes is linked to their ability to invade cells, replicate intracellularly within epithelial cells, produce lipopolysaccharide coats, and release toxins. These toxins include endotoxins, which induce fever; enterotoxins, which may not cause diarrhea but reduce epithelial cell secretory responses; and cytotoxins responsible for intestinal epithelial cell damage by inhibiting protein synthesis and chelating iron.
Several other virulence factors contribute to disease establishment, including adhesion pili, surface polysaccharide O antigens, flagellar H antigens, fimbriae production, colicin and porin production, and resistance to the lethal effects of large plasmids (30-60 megadaltons). Systemic disease arises from bacterial survival within macrophages, with Salmonella pathogenicity islands (SPI) and virulence plasmids playing pivotal roles in virulence.
Salmonella exhibits acid tolerance, surviving gastric acid and barrier passage. Acid shock proteins protect against acid stress, with certain food matrices offering protection, especially when high-fat foods are consumed.
Salmonella adheres to mucosa through fimbrial attachment in the intestine, inducing cell membrane ruffling to facilitate uptake into non-phagocytic cells. The Type III secretion system (TTSS), present in all S. enterica serotypes, transports virulence factors via a needle-like structure, altering cellular secretory pathways, ion balance, and causing inflammation and neutrophil recruitment, ultimately leading to diarrhea. Effector proteins also play roles in the formation of Salmonella-induced filaments, aiding intracellular replication and protecting intracellular organisms from host cell bactericidal compounds like reactive oxygen intermediates. Certain virulence genes are crucial for intracellular survival and invasion.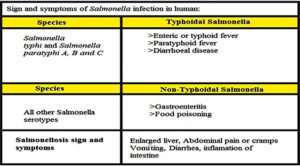
Salmonella infection results in a spectrum of clinical outcomes, including enteric fever (typhoid fever and paratyphoid fever), gastroenteritis, food poisoning, abdominal pain, vomiting, and diarrhea.
Salmonella infection is a global concern, affecting both developing and developed countries. It disproportionately impacts children and young adults aged 5-20 years. Epidemiology varies depending on the Salmonella serotype involved. S. Typhi and S. Paratyphi primarily cause chronic or severe disease (typhoid fever) in humans but do not affect non-human hosts. Typhoid disease is especially prevalent in medically underserved communities. In contrast, non-typhoidal Salmonella infections tend to be self-limiting and affect communities worldwide.
Preventing Salmonella infection necessitates a multifaceted approach that incorporates several key measures. First and foremost, proper cooking is essential. Ensuring that food is cooked thoroughly is critical to effectively kill any Salmonella bacteria that may be present.
Safe food handling practices should also be diligently followed. This includes measures such as avoiding cross-contamination, storing food at proper temperatures, and practicing good hygiene when preparing and serving food.
Maintaining high standards of sanitation is another crucial element of Salmonella prevention. This involves keeping food preparation areas clean, regularly disinfecting surfaces, and ensuring the proper disposal of waste.
In regions where vaccinations against Salmonella are available, considering vaccination can be a proactive step towards preventing infection.
Hand hygiene plays a pivotal role in preventing Salmonella transmission. It’s imperative to wash hands thoroughly after handling animals, especially those known to carry Salmonella, as well as after working with meat products.
Lastly, access to safe water sources is paramount. Ensuring that drinking water is free from contamination is essential for preventing waterborne transmission of Salmonella.
Incorporating these prevention measures into daily practices can significantly reduce the risk of Salmonella infection and promote overall public health.
By understanding the pathogenesis and implementing preventive measures, we can reduce the burden of Salmonella infections in both human and animal populations.






